So it has been a while since I have written a blog post. There is so much I want to say but instead of having word vomit just in the blog post I will try to spread it out over a few post. However the one topic I want to discuss is a DAT brain. I have not only come back to the DAT to finish out my last 2 classes and Graduate in December. I have also transitioned from the industrial setting back to the traditional collegiate athletic setting.
The industrial setting, though I learned a lot, is not for me. I felt very restrictive in what I was allowed to do with my patients. For those who don’t know much about the industrial setting, you primarly have to follow OSHA’s guidelines for first aid- ICE/ heat, wound care, hydration, stretching( that are predetermined and job specific), and massage. There is a little more to it, but that is the gist of what I was allowed to do. So many of the treatments I did were “massage.” Now I am once again in a traditional collegiate setting I feel free… but lost. I sort of forgot how to think like a DATer. I know, I know, it should be in my blood and I should always think like a DATer, but I noticed that I was reverting back to stretch/ strengthen when I couldn’t figure something out right away. That is until I had a patient present with low back pain. I love low back pain, especially if it stems from the sacrum. However, this patient was not a typical low back case, and I didn’t relize that until I had him squat. When I first evaluated him, I had him perform the “normal” back movements- flexion/ extension, rotation, lateral flexion, hip flexion. I did notice that his flexion was not a fluid motion. His pain was localized to the right side so when he tried to touch his toes he laterally flexed to the right and also began to bend his knee. I thought this awkward movement was due to his pain. Then I asked him to do a squat, which is pictured below. As he was squatting, I thought to myself – “how does someone lack this much mobility in his body and still be coach’s “top recruit?”, as well as that must be very painful.” But then I had a mini freak out. How do I help him correct all of these dysfunctional movements? Where do I start?
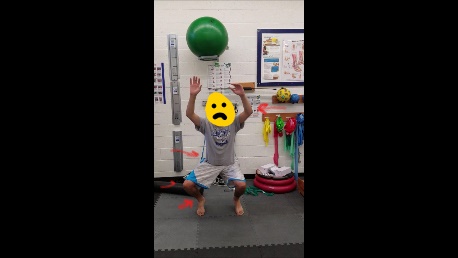
I didn’t have my SFMA cheat sheets, so I just used a best guess from the dysfucntional flexion and squat, that he had a flexion stability motor control dysfunction… so that is where I started. We began with rolling patterns and continued to quadruped band work. I also worked with weight bearing stability and engaging his core, glutes, and breathing pattern. I was focused on treating the back pain first to get him back to practice and not all of his dysfunction. Now my DAT brain kicked in and I know that his back pain can be stemming from his ankle dysfunctions. Therefore I am planning on taking him through a full SFMA check up to see what else we need to improve as well, but I am glad to say from the work we have done his DPAS, NRS, and HSAQ have all improved. ( will proved the scores once I return to work)
Details have never been one of my strong points. One of my goals for this semester is to improve my attention to details, as well as reporting the details. So I apologize for the lack of detail about his patient I will fill in with specific exercises and PRO’s when I am back in the office.
My DAT brain is slowing reloading and that makes me very happy and excited. I have two assistants who are great and also very excited to learn the paradigms I know. A few times they have asked me to teach them something, which I think is triggering my DAT brain even more. I am excited to see how much I can teach them by just working in the same clinic.

Emily, thanks for sharing this post. I completely understand where you are coming from with your mindset. It can be very easy to revert to old habits. The DAT philosophy will come back faster than you think. After reading through your description of the case of LBP the first thing that popped into my head was MYK. If you are familiar with MYK I would recommend doing a postural assessment, seeing which nerve roots are most affected and then begin to treat one at a time. It may be advantageous, depending on how much time you have, to reassess after each treatment. If you don’t have that kind of time, just treat through the most affected nerve paths. I truly believe you will have great success corrected any postural abnormalities which will hopefully lead to pain-free functional movement. Keep us posted.
Josh,
I actually only know and have the materials for the MYK of upper body. I never learned the lower half. I may loom I to the materials, just for this patient.
Hello Emily, Can you update this post when you complete the full SFMA check up?